Diabetic foot ulcer (DFU) is an open sore or a wound that is commonly noted in individuals with uncontrolled diabetes mellitus because of repeated trauma and pressure to the area. It is a chronic / long-standing condition, which most commonly occurs due to underlying neuropathy or peripheral vascular disease, and is worsened by poor foot care.
Facts about diabetic foot ulcer
DFU is noted in 6.3 % of the world's population with North America having the highest prevalence that has been estimated at 13 %.
In Asia, 5.5 % of diabetic patients go on to develop DFUs.
In India, the prevalence of diabetic foot ulcer is 11.6%1.
The lifetime risk of a person with diabetes developing a foot ulcer could be as high as 25 %; this risk is elevated in the presence of other risk factors. Approximately 85 % of lower limb amputations in patients with diabetes are preceded by foot ulcerations.
Patients with type 2 diabetes mellitus are at a greater risk of foot ulcerations when compared to patients with type 1 diabetes mellitus (6.4 % vs 5.5 %) .
Elderly patients and those with a history of long-standing diabetes mellitus are at an elevated risk. The risk of DFUs is significantly high in the presence of other comorbid conditions such as high blood pressure, kidney disease, or cerebrovascular disease.
Approximately 24% of DFUs finally lead to limb amputations if sufficient precautionary measures are not instituted.
Diabetic foot was more prevalent in males than in females, and more prevalent in type 2 diabetic foot patients than in type 1 diabetic foot patients. The patients with diabetic foot were older, had a lower body mass index, longer diabetic duration, and had more hypertension, diabetic retinopathy, and smoking history than patients without diabetic foot.
Risk factors for the development of diabetic foot ulcer
Several risk factors are responsible for the development of DFUs including injuries, systemic conditions or repeated trauma / stress. These have been listed under Table 1.
|
Risk Factors for Diabetic Foot Ulcers
|
|
Age - Over 55 years
Body mass index > 25 kg/m2
-Co-morbidities such as high blood pressure, kidney disease, cerebrovascular disorders like
Smoking
Duration of diabetes in years >3 years
Poor compliance with anti-diabetic therapy
Presence of nail pathology such as fissures or callus
Presence of existing disability or deformity such as clawing of toes, high arch, and subluxed metatarsophalangeal joints, leading to excess pressure
Absent pulses
Peripheral neuropathy
Impaired immune function
Poor wound healing
Frequent unattended injuries to the area of the foot
Walking barefoot leading or poor footware which inadequately protects the skin from high pressure and shear forces
Dry skin type
Impaired vision
History of foot ulcer or lower extremity amputation
|
Table 1: Risk Factors for Diabetic Foot Ulcers
|
How does the ulcer start and look like?
The diabetic foot ulcer develops in stages. At the first stage, there will be no visible symptoms. You may only feel pain sensations or there will be no symptoms at all depending on your degree of neuropathy.
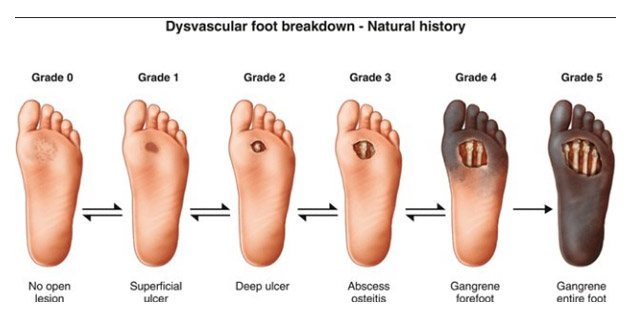
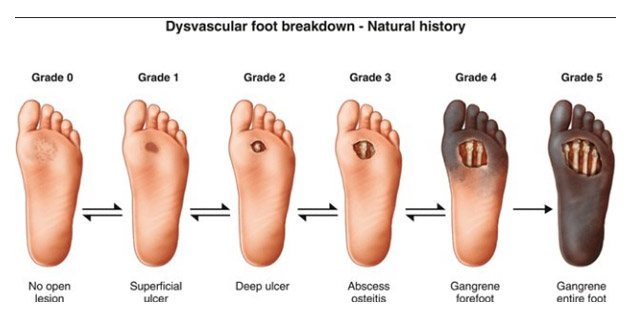
The grades of DFU are elaborated below:
| Grade 0 - Foot symptoms like pain, only |
| Grade 1 - Superficial ulcers |
| Grade 2 - Deep ulcers |
| Grade 3 - Ulcer with bone involvement |
| Grade 4 - Forefoot gangrene |
| Grade 5 - Full foot gangrene |
You and your health care provider need to look for these signs and symptoms so that DFU can be managed before it reaches a terminal stage requiring foot amputation.
The starting point of DFU will be seen as a minor wound in the form of a blister, injury, or a callus, which you may notice upon routine foot examination.
You must look out for small cuts due to walking bare feet or pressure sores developed due to wearing poorly fitted shoes. If you note that such types of injuries are taking a longer time to heal, early stage of DFU can be suspected.
Another early sign indicating that you are at an early stage of DFU is lack of foot sensations. You may feel that your foot is numb to pain and temperature changes, and pressure sensations due to small injuries go unnoticed.
Unexplained injuries in the area of the foot are one of the most common manifestations at the initial grades. This happens because the sensory nerves do not function optimally and thus, fail to transmit proper messages, and signals between the brain and the affected foot.
At grade 3 or deep ulcerations, there will be an evidence of the involvement of deeper tissue structures such tendons or muscles. At this stage, there is also a severe risk of foot infections, which will be confirmed by your physician on the basis of lab investigations.
Gram-positive bacteria, gram-negative bacteria, and anaerobes are the most common infectious agents for DFUs.
The infection then gradually starts spreading to your bone and marrow structures. Your physician will be able to diagnose this by physical examination and you may also be able to note white bony structure on self-examination. At this stage, walking and mobility issues start becoming apparent.
Presence of deep ulcerations increases your risk of osteomyelitis , which will need to be confirmed with the help of an X ray examination and a biopsy. Presence of discharging sinus and sausage-like appearance of the toe are the clinical signs of osteomyelitis that must be looked out for, and immediate medical assistance must be sought.
At grade 4 and 5, the presence of gangrene or dead tissue is evident. This is noted as blackish to bluish discolouration of the skin along with the presence of severe pain or numbness and foul smelling discharge. At this stage, amputation of the affected area of the foot is necessary to cease the gangrenous spread.

https://woundreference.com/app/topic?id=patient-education-diabetic-foot-ulcer
https://vitamindwiki.com/Diabetic+Foot+Ulcer+3.2+X+or+3.6+X+more+likely+if+low+vitamin+D+%E2%80%93+meta-analyses+2019
Figure 1: Stages of Diabetic Foot Ulcer
What to do if I see signs of a foot ulcer developing?
As soon as you notice the symptoms of a diabetic foot ulcer, the first thing you must do is to consult a specialist. You must consult with your specialist doctor who will conduct the necessary tests and plan your multi-disciplinary care. You must have understood how serious untreated ulcers can be, so, do not delay the treatment at any cost.
Other than this, it is also important that you engage in regular foot examinations. If at all you notice any small symptom, it is essential that you pay attention to it and inform your physician of even the minutest changes in its appearances.
If you seek treatment in time, debridement and infection control may be enough to manage the symptoms. In the process of debridement, dead and infected tissues from the wound by a team of experienced medical professionals who prescribe suitable oral antibiotics or topical ointments.
Even after the successful treatment of ulcers, it is essential that you engage in foot examination and regularly visit your physician for follow up investigations because DFUs possess a high risk of recurrence.
References:
1. Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Annals of medicine. 2017 Feb 17;49(2):106-16.
2. Packer CF, Manna B. Diabetic Ulcer. InStatPearls [Internet] 2019 Mar 24. StatPearls Publishing.
3. Alex R, Ratnaraj B, Winston B, Devakiruba DN, Samuel C, John J, Mohan VR, Prasad JH, Jacob KS. Risk factors for foot ulcers in patients with diabetes mellitus-a short report from vellore, South India. Indian journal of community medicine: official publication of Indian Association of Preventive & Social Medicine. 2010 Jan;35(1):183
4. Armstrong DG, Lavery LA. Diabetic foot ulcers: prevention, diagnosis and classification. American family physician. 1998 Mar 15;57(6):1325.
5. Pendsey SP. Understanding diabetic foot. International journal of diabetes in developing countries. 2010 Apr;30(2):75
6. Oliver, T. I., & Mutluoglu, M. (2019). Diabetic foot ulcer. In StatPearls [Internet]. StatPearls Publishing